Association between diagnosis-to-limb revascularization time and clinical outcomes in outpatients with chronic limb-threatening ischemia: insights from the CLIPPER cohort
Selected in JAHA by Delphine Donzel
Peripheral artery disease can lead to limb-threatening ischemia, yet many patients face delays in revascularization, increasing the risk of major amputation. This study addresses the urgency of reducing these delays.
References:
Authors: Alexander C. Fanaroff, Elias J. Dayoub, Lin Yang, Kaitlyn Schultz, Omar I. Ramadan, Grace J. Wang, Scott M. Damrauer, Elizabeth A. Genovese, Eric A. Secemsky, Sahil A. Parikh, Ashwin S. Nathan, Maureen P. Kohi, Mitchell D. Weinberg, Michael R. Jaff, Peter W. Groeneveld, and Jay S. Giri, MD, MPH
Reference: J Am Heart Assoc. 2024;13:e033898.
DOI: 10.1161/JAHA.123.033898
Read the abstractObjectives:
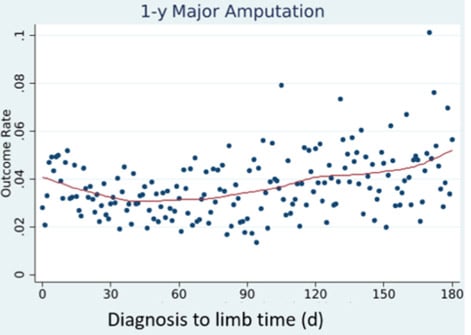
To describe the distribution of time from CLTI diagnosis to outpatient endovascular revascularisation (D2L time) and its association with clinical outcomes
Population:
99,221 patients with fee-for-services Medicare who underwent endovascular revascularisation within 6 months of CLTI diagnosis
Endpoints:
All-cause death and/or major lower extremity amputation in the 1 year after lower extremity revascularization
Outcomes and conclusion:
A delay of > 30 days from CLTI diagnosis to outpatient lower extremity endovascular revascularisation was associated with an increased risk of major lower extremity amputation.
Compared with CLTI patients who did not undergo out- patient endovascular revascularization, patients who underwent outpatient revascularization were younger (74.9 versus 75.4years), less often Black individuals (13.4% versus 14.8%), and less often women (44.4% versus 48.7%); they had a higher prevalence of heart failure, obesity, and depression, but similar prevalence of diabetes, hypertension, and chronic kidney disease.
Get the latest clinical cases and breaking news delivered straight to your inbox!


Comments: