Clinical outcomes of transradial vs non-transradial aortoiliac endovascular therapy: COMFORT registry
Selected in JACC: Cardiovascular Interventions by Myriam Afifi
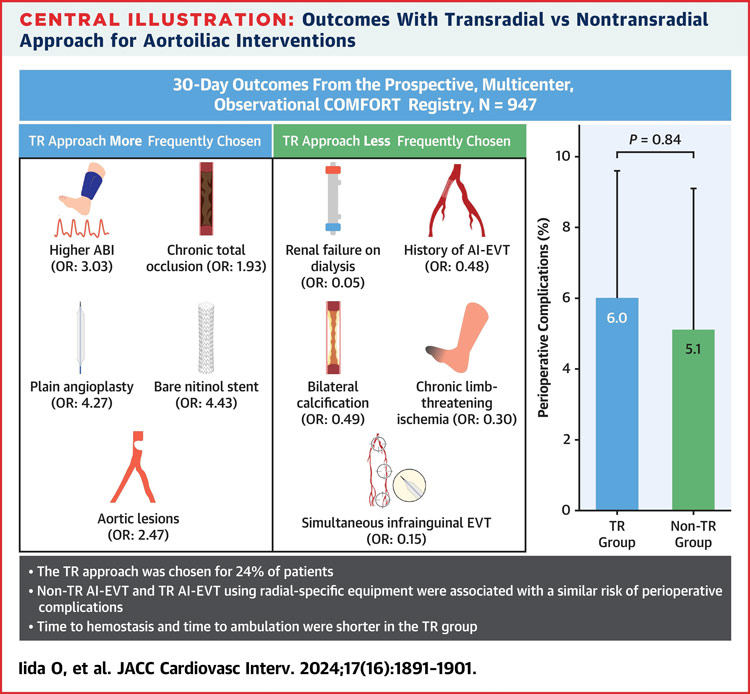
Endovascular revascularisation is the first choice for symptomatic PAD, but traditional transfemoral access can be challenging. Transradial access is emerging as a less invasive alternative. This study examines the criteria for selecting transradial access and its outcomes in aorto-iliac revascularisation for PAD patients.
References:
Authors: Osamu Iida, Mitsuyoshi Takahara, Masahiko Fujihara, Naoko Higashino, Naoki Hayakawa, Kazunori Horie, Yoshito Yamamoto, Amane Kozuki, Kenji Suzuki, Norihiko Shinozaki, Hiroyoshi Yokoi, Shinsuke Nanto, Yoshiharu Higuchi, the COMFORT Investigators, and Masato Nakamura
Reference: J Am Coll Cardiol Intv. 2024 Aug, 17 (16) 1891–1901
DOI: 10.1016/j.jcin.2024.06.002
Read the abstractObjectives:
To investigate the perioperative outcomes of the TR approach in patients undergoing aortoiliac endovascular therapy for symptomatic peripheral artery disease.
Population:
947 patients with symptomatic peripheral artery disease undergoing aortoiliac endovascular therapy between January 2021 and June 2023. Selection of access was determined at the discretion of vascular specialists.
Endpoints:
The primary outcome was perioperative complications. The secondary outcomes included residual stenosis > 30 %, time to hemostasis, time to ambulation, 30-day patency, and 30-day limb symptoms.
Outcomes and conclusion:
Non-TR and TR aortoiliac endovascular therapy using radial-specific equipment were associated with a non-inferior risk of perioperative complications. The TR approach seemed to shorten the time required for hemostasis and ambulation.
Get the latest clinical cases and breaking news delivered straight to your inbox!


Comments:
Largest study on endovascular revascularisation via transradial access
Reflects current practice (operator’s choice)