Delays to revascularisation and outcomes of non-elective admissions for chronic limb threatening ischaemia: a UK population based cohort study
Selected in ESVS Journal by Jana Hammoud
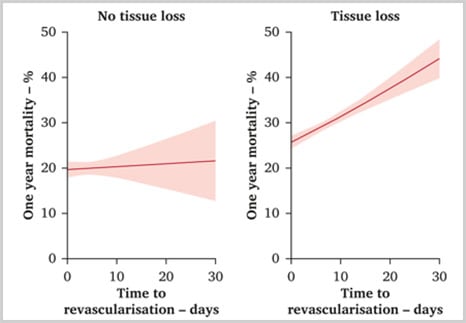
This study evaluates the impact of revascularisation timing on mortality and major amputation rates in emergency admissions for chronic limb-threatening ischaemia (CLTI). Analysis of over 10,000 patients revealed that delays in revascularisation, particularly in those with tissue loss, were associated with higher one-year mortality rates, highlighting the importance of timely intervention for improving patient outcomes.
References:
Authors: Panagiota Birmpili, Qiuju Li, Amundeep S. Johal, Eleanor Atkins, Sam Waton, Arun D. Pherwani, Robin Williams, Ian Chetter, Jonathan R. Boyle, and David A. Cromwell
Reference: Published online December 24, 2024
DOI: 10.1016/j.ejvs.2024.12.038
Read the abstractObjective:
The aim of this study was to evaluate the relationship between the timing of infrainguinal revascularisation and major amputation and mortality rates at one year for patients admitted to hospital as emergencies with CLTI.
Study:
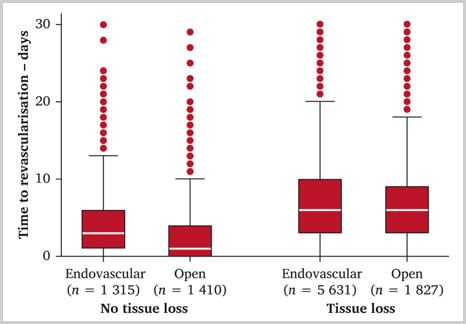
Retrospective scanning of the Hospital Episode Statistics (HES) Admitted Patient Care (APC) database between 2017 and 2019 for patients with CLTI who underwent infra-inguinal revascularisation and the impact of timing on death and major amputation.
Population:
10,183 patients were identified with CLTI admitted as emergencies for infra-inguinal revascularisation.
Endpoint:
Primary outcome was death at one year, and the secondary outcome was ipsilateral major amputation at one year after the index revascularisation procedure. Death and major amputation were also examined as time to event variables.
Outcomes and conclusion:
Patients undergoing infrainguinal revascularisation during non-elective admissions for CLTI have high one year major amputation and mortality rates. Longer time from admission to revascularisation was independently associated with a higher mortality rate in patients with tissue loss, but not in those without.
Get the latest clinical cases and breaking news delivered straight to your inbox!


Comments
Patients admitted as emergencies for critical limb ischemia (CLI):
-> High mortality due to emergency admissions
-> No link between delay and major amputation, as severity and disease progression have a bigger impact
-> Patients treated later due to pre-operative treatments (e.g., antibiotics, optimisation, imaging) and hospital constraints
Strengths:
Weaknesses: