Outcomes following arteriovenous fistula creation in Medicare beneficiaries with end-stage kidney disease
Selected in The American Journal of Cardiology by Perrine Darpy
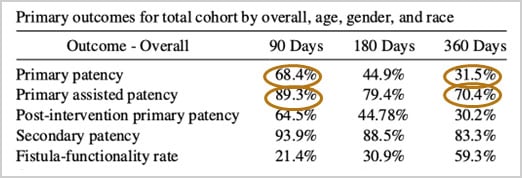
This recent cohort study analysed arteriovenous fistula (AVF) outcomes in U.S. Medicare beneficiaries with end-stage kidney disease (ESKD). The findings revealed that primary AVF patency rates at one year were lower than those reported in clinical trials. Notably, women and Black patients experienced disproportionately lower patency rates, even after adjusting for other factors, while age did not significantly influence outcomes.
References:
Authors: Nathan W. Kong, Joseph M. Kim, Anna K. Krawisz, Patrick Heindel, Archana Tale, Yang Song, Jeffrey L. Weinstein, Mohamad A. Hussain, and Eric A. Secemsky
Reference: Am J Cardiology 2025 Jan 1:234:79-86
DOI: 10.1016/j.amjcard.2024.10.006. Epub 2024 Oct 22
Read the abstractObjective:
The aim of this analysis was to characterize contemporary longitudinal patency and adverse events in a real-world population of patients with end-stage kidney disease (ESKD) in the United States.
Study:
The studied cohort included all patients ensured by Medicare fee-for-service (FFS) who underwent AVF creation from January 1, 2017 to June 30, 2019
Population:
Patients who underwent AVF creation in the United States and who benefit from Medicaid or Medicare Service
Endpoint:
Primary patency at 1 year.
Outcomes and conclusion:
The primary patency of AVFs in Medicare beneficiaries was small, particularly when compared with previous studies in trial settings.
Second, age did not seem to be a major contributor to AVF patency.
Last, women and Black patients had disproportionately lower rates of AVF patency, even after multivariable adjustment.
Get the latest clinical cases and breaking news delivered straight to your inbox!


Comments:
The study reports a primary patency rate of 31 % at one year, notably lower than the 60 % observed in studies from 1970 to 2012. This decline may be attributed to changes in patient demographics undergoing arteriovenous fistula (AVF) creation.
While proactive maturation techniques, such as angioplasty-assisted maturation, have improved the one-year assisted primary patency rate to 70.4 %, the post-intervention patency remains low at 30.2 %, leading to a cycle of multiple interventions, averaging 2.61 per patient-year.
Study limitations:
These limitations suggest that the findings may not be generalizable to all patient populations. Further research is needed to address these gaps and improve AVF patency outcomes.