Popliteal access for iliofemoral occlusive disease in the office-based catheter laboratory
Selected in Journal of Vascular Surgery by Xavier Devoisin
This retrospective single-center study evaluates the safety and efficacy of popliteal access for endovascular treatment of iliofemoral occlusive disease in an outpatient setting. Among 27 procedures, revascularisation was successful in 92.5 % of cases, with no major adverse events and a low reintervention rate at 3 and 12 months. The findings support popliteal access as a safe and effective alternative for complex iliofemoral disease in outpatient care.
References:
Authors: Hani Shennib, Emily Teribery, Amanda Evans, and Victor Huerta
Reference: J Vasc Sur. 2025 Jan;81(1):165-171. doi: 10.1016/j.jvs.2024.08.055. Epub 2024 Aug 30.
DOI: DOI: 10.1016/j.jvs.2024.08.055
Read the abstractObjective:
To evaluate the safety and efficacy of popliteal access for endovascular treatment of iliofemoral occlusive arterial disease in an outpatient setting.
Study:
Single-center retrospective cohort
Outcomes and conclusion:
27 procedures using popliteal access for femoral and iliac artery occlusions. Revascularisation success in 92.5 % of cases.
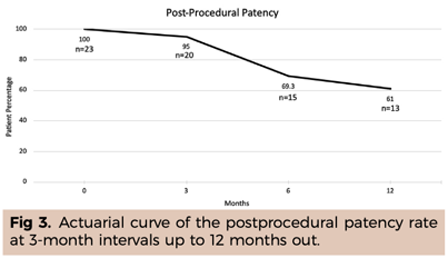
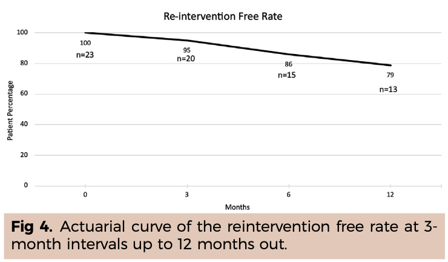
No major adverse events observed, with no reintervention at 3 months in 95 % of cases and at 12 months in 79 % of cases.
Popliteal access for complex iliofemoral disease is safe and effective and should be considered a viable alternative in outpatient care.
Get the latest clinical cases and breaking news delivered straight to your inbox!


Comments:
Disadvantages:
Advantages:
Clinical insights:
Procedure efficiency: