Presence of atherosclerosis in multiple arterial beds is associated with increased mortality in patients undergoing endovascular aortic aneurysm repair
Selected in ESVS Journal by Perrine Darpy
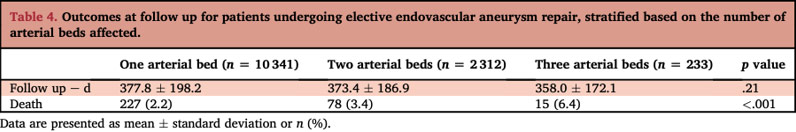
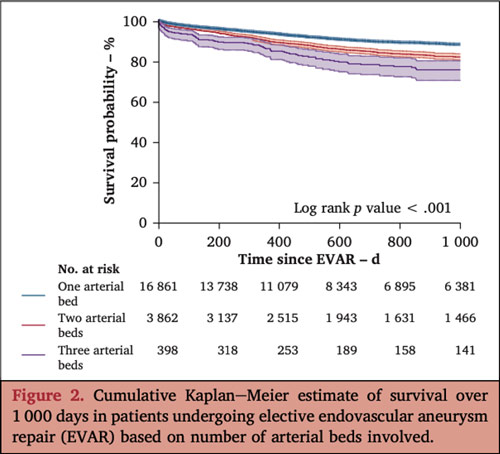
This retrospective study aimed to quantify the impact of atherosclerotic disease burden on mortality and morbidity in patients undergoing elective endovascular aneurysm repair (EVAR) for aneurysmal disease. The research focused on patients who underwent EVAR between 2012 and 2022, assessing the presence of atherosclerosis in multiple arterial beds and its association with peri-operative outcomes, specifically death and major adverse cardiovascular events (MACE).
References:
Authors: Molly Ratner, Heepeel Chang, Caron B. Rockman, Benjamin J. Pearce, Jeffrey J. Siracuse, Jae S. Cho, Neal Cayne, Thomas Maldonado, Virendra Patel, Karan Garg
Reference: Eur J Vasc Endovasc Surg Volume 69, Issue 1, p81-87, January 2025
DOI: DOI: 10.1016/j.ejvs.2024.10.004
Read the abstractObjective:
To quantify the effects of atherosclerotic disease burden on mortality and morbidity in patients undergoing elective endovascular aneurysm repair (EVAR) for aneurysmal disease.
Study:
This retrospective study used the Vascular Quality Initiative (VQI) database from the Society for Vascular Surgery (SVS).
Population:
Patients who underwent EVAR between 2012 and 2022.
Endpoints:
Death and MACE.
Outcomes and conclusion:
In patients undergoing EVAR, those with polyvascular disease more frequently experienced peri-operative MACE and death. Moreover, a gradation of risk was observed with the increasing number of arterial beds involved. Patients with polyvascular disease should be considered high risk and managed accordingly.
Get the latest clinical cases and breaking news delivered straight to your inbox!


Comments:
Study limitations: